Blogs by Topic:
Why Physical therapy or Occupational therapy:
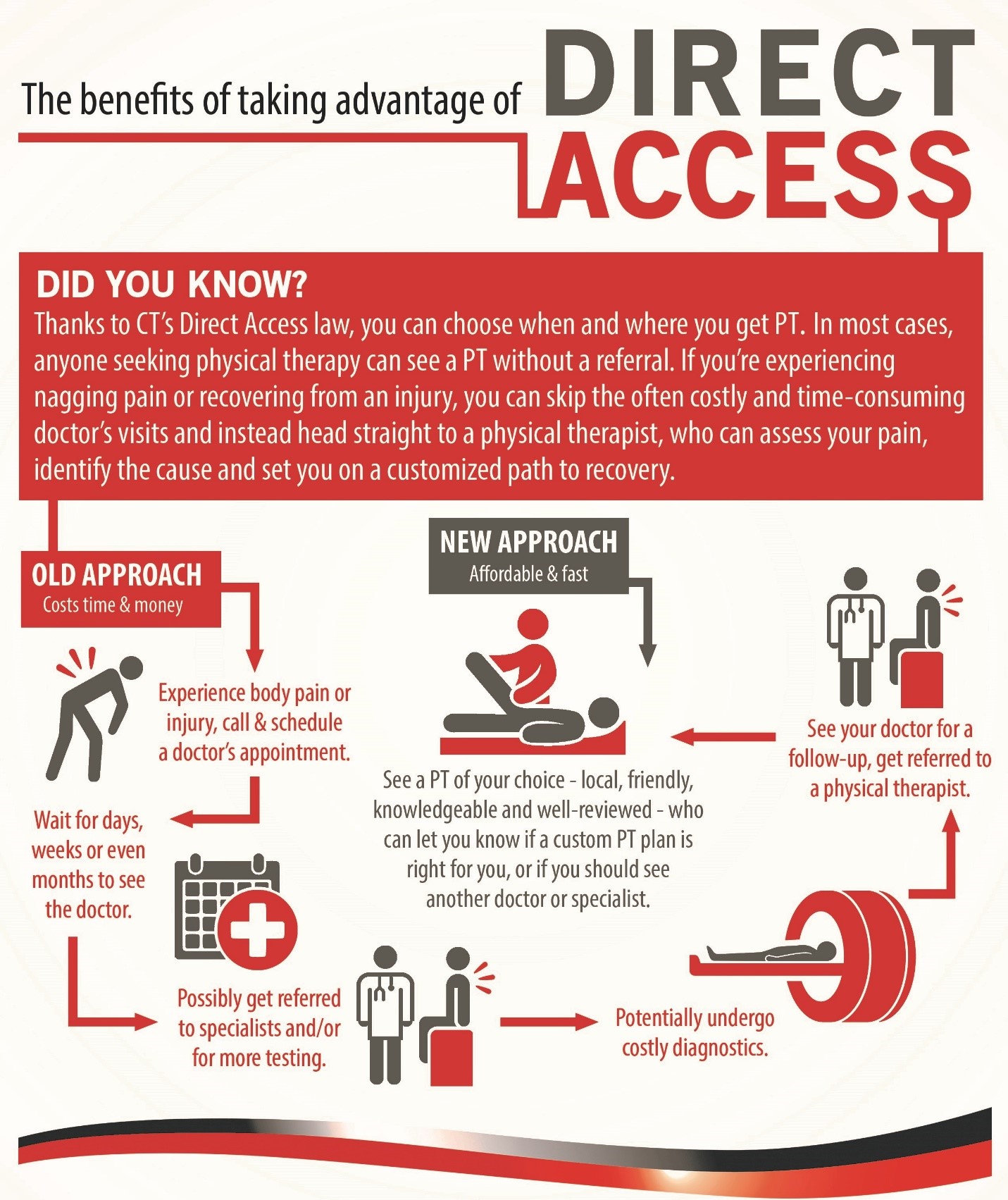
Choose PT First to save time and money
Are you a smart consumer of Healthcare?
Conditions:
Pain relief without medication
What you need to know about arthritis
Your x-rays and MRIs show us the wrinkles on the inside
A new way to Treat Fibromyalgia
Share your goals; they’re important to us!
Back and Neck Pain:
Best way to get rid of back and neck pain
Essential Exercises for Back pain
Can PT help with Headaches/ Migraines?
Can PT help Back Pain? What we learned from Starbucks
Shoulder:
Prevent and Treat Shoulder Pain
Elbow:
Elbow Tendonitis, a.k.a Tennis Elbow
Wrist/ Hand:
Foot/Ankle:
Why Flip Flops may not be your best option
Pelvic Health:
What is Pelvic Health Physical Therapy
How to stay active during pregnancy
Surgery:
Tips & Tricks to Prepare for Surgery
Stronger going into Surgery, Stronger Coming out.
Common Interventions:
Should I be Stretching or Strengthening?
Seasonal:
A PTs Guide to Snow Shoveling Safety
Winter Safety in Industry: Navigating Cold Conditions with Confidence
Finding your balance in winter
Keeping your arms and hands safe in the Winter
Protecting your joints with summer activities
Information for all of our Green Thumbs
Athletics:
Preventing Pickleball Injuries
Could early specialization be the problem?
Concussion:
Everything you need to know about Concussions
Importance of Baseline Concussion Testing
Running:
Return to Running, Spring Edition
Injury Prevention, do shoes matter?
Orchestra and Performing Arts:
Industrial medicine:
Impact of Athletic Trainers in Industrial Care
Lifting Basics Part 1: Warm-ups, Cool-downs, Strengthening
Lifting Basics Part 2: Safe Lifting Practices ALL Workers Should Know.
Lifting Basics Part 3: Exploring Safe and Effective Lifting Techniques
Lifting Basics Part 4: Effective Ways to Safely Move Objects
Tactical Medicine:
Return to Work Assessment for an Injured Police Officer
Police Support Staff Person of the Year
Things we learned from participating in a mass-casualty simulation
Office:
Getting more activity during your workday
Decrease Fatigue and Reduce Stiffness
Direct Contracting:
Our role in providing exceptional care to the employees of local School Districts
Wellness:
Importance of physical activity
Why you need a PT on your team
The 4 P’s of Energy Conservation
Hidden Aches and Pains caused by Cell Phones
How to decrease the aches and pains brought on by using your phone
Movement Vital Sign, what is that?
You’re never too old to strength train
Improve your mood with exercise, especially during the holidays
Importance of Building Strength
Meet the Team:
The 4 P's of Energy Conservation
The 4 P’s of Energy Conservation
Laura Johnson, PT, DPT
Has it been exhausting for you to complete your typical morning routine, or maybe you are having shortness of breath while grocery shopping? When individuals have a diagnosis of Chronic Obstructive Pulmonary Disease (COPD), Multiple Sclerosis (MS), or Congestive Heart Failure (CHF), or are recovering from a recent illness or surgery, it can be difficult to complete daily chores due to fatigue and decreased activity tolerance. Your lungs and heart may not be working as efficiently as they should, so it is important to conserve energy throughout the day.
In order to succeed, there are 4 simple steps to consider, and we are going to refer to these as the 4 P’s of Energy Conservation
1. PRIORITIZE: Decide what needs to be done today, and what can wait for a later date. Try to scatter your household chores throughout the week. One day for laundry, next day for vacuuming and another day for grocery shopping. If you are partaking in a social engagement, plan to skip some daily activities to reserve some energy before the fun begins! A good quality rest period each day is best!
2. PLAN: Plan ahead to avoid extra trips. Gather supplies and equipment needed before starting an activity. For example, before showering, make sure your towel, clothes and necessary daily items are all located in the bathroom area. Also have a chair available to provide yourself a seated rest break if needed. Another technique is to plan to alternate heavy and light tasks. Find a good balance between work, rest and leisure.
3. PACE: Slow and steady pace, never rushing! Some individuals try to complete as many tasks as possible, as quickly as possible. Unfortunately, this leads to complete exhaustion, and inability to perform tasks later in the day. This can also lead to a greater chance of falls due to increased fatigue: We all know a fall can be extremely traumatic. Plan to rest before you feel tired. Provide yourself with enough time to take short, frequent rest breaks.
4. POSITION: Think about your body position while completing tasks throughout the day. Bending and reaching can cause fatigue and shortness of breath. There is adaptive equipment available to make some daily tasks less stressful on your body. Examples are: 1) Use a reacher to grasp the cleaning supplies in the low cupboard, 2) Use elastic shoe laces to avoid bending over to tie your shoes, or 3) Use a sock aid to get your socks or compression stockings on. Eliminating some strain when bending or reaching will allow your lungs to expand more fully, which in turn helps get more oxygen into the body.
Conserving your energy can allow you to complete the tasks you want to complete throughout the day. You do not want to run out of energy before the day is through and we definitely do not want you to entirely stop your activity for constant rest. Get moving, but move smarter!
If you’re interested in developing an energy conservation plan specific to your needs, contact one of our physical or occupational therapists today to discuss it further.
Click here for a complete list of locations.
Are You a Smart Consumer of Healthcare?
ARE YOU A SMART CONSUMER OF HEALTHCARE
Think about the last time you made a big purchase, say $1,000 or more. Did you go out and buy the first thing you saw? Take one recommendation from somebody? Or did you research it, learn some things, compare it to other options, and select something that was right for you? Most people tend to be educated and research large purchases like cars, televisions, or the newest iphone. So why do we so often fail to do this with healthcare?
By becoming more educated healthcare consumers we can go from passive patients who take the first recommendation that comes from a practitioner to an active consumer who weighs options and makes choices. Here are some questions to talk through with your practitioner the next time a healthcare decision comes up.
WHAT ARE THE BENEFITS OR EXPECTED RESULTS?
When a treatment or procedure is recommended, the patient often assumes that it will make them "better." But what the patient expects and what the healthcare provider expects are often two different things. For example, a patient having back surgery expects to be pain free after surgery. The surgeon probably doesn't expect that to happen. Outcomes from back surgeries are terrible. A large study of 1450 patients in the Ohio worker's comp system showed that after 2 years 26% of patients who had surgery returned to work. Compare that to 67% of patients who didn't have surgery. There was also a 41% increase in the use of painkillers in the surgical group.
WHAT ARE THE RISKS AND DOWNSIDES?
Patients want to hear about the benefits of a treatment, but they often don't ask or care about the risks. To be an educated consumer, you need to. If one treatment has a 3% edge over another, but has a high risk of making you itchy or causing frequent headaches, do you want it? Going back to the back surgery study from before, the researchers found a 1 in 4 chance of a repeat surgery and a 1 in 3 chance of a major complication. With surgery you risk infection, blood clots, complications with anesthesia, and a whole host of other things. These risks need compared with other treatments. In the case of back pain, physical therapy is a valid alternative with a much lower risk profile. You might have some soreness with physical therapy, you might sweat some and be challenged with exercise, but the risks of PT compared to surgery are minimal.
WHAT ARE THE ALTERNATIVES?
Don't feel bad asking about alternative treatments. If you were looking at a certain car you wouldn't go out and just buy it. You'd at least consider the competitors and probably even test drive them. You should at least look at the other options in healthcare too. Maybe the first recommendation that your practitioner makes is the right one for you, but if you don't consider the alternatives you'll never really know.
WHY THIS TREATMENT OVER THE OTHER ONES?
This is the question where the rubber meets the road. You've learned about all the options, now you can see if your practitioner is balancing the risks and benefits to make the right choice for you. Staying with the back pain example, research shows that more than 40% of people who seek care for back pain will not receive a treatment of known effectiveness. Back pain is also the #1 reason for opioid prescriptions, despite a 2016 recommendation from the CDC to avoid prescribing opioids for back pain, and opt for non-drug treatments like physical therapy. By asking for the rationale and carefully weighing options, you can avoid being one of the people who gets an ineffective treatment.
WHAT'S IT COST?
This last question is becoming more important as patients bear an increasing share of the cost of healthcare. Even if you don't have a high deductible plan or hefty co-pays, by being financially responsible today, you'll probably see smaller price increases in your premiums down the road. That back surgery that we've been talking about? It'll likely cost between $60,000 and $80,000. So if we put the whole picture together, a patient who takes the first recommendation for surgery will have a $60,000 procedure that leads to a higher risk of disability, and a higher risk of long term painkiller use, while risking infection, and blood clots. Don't forget the 25% chance that you'll get to do it all again in a repeat surgery. Seems like a bad deal. An educated consumer would learn that physical therapy is a viable alternative to surgery with comparable outcomes, much less risk and lower cost. In fact, a large study of 122,723 subjects showed that people with back pain who got physical therapy in the first 14 days lowered their healthcare costs by 60%. It's easy to see why bargain shoppers love PT!
Hidden Orthopedic Cell Phone Dangers
Your Smart Phone Could Be Rapidly Aging Your Spine
Chances are that you probably haven’t given much thought to how your neck and back are faring in the era of the smart phone, but studies show that you most certainly should. It’s practically a reflex these days to pull out our smart phones when we’re standing in line, sitting at the airport or riding the subway. And while it’s great that we rarely need to venture beyond our pockets for entertainment, our bodies are beginning to retaliate—and mourn the pre-texting days.
So, what exactly are these contemporary conveniences doing to our bodies? A surgeon-led study that published in Surgical Technology International assessed what impact surgeons’ head and neck posture during surgery—a posture similar to that of smart-phone texters—has on their cervical spines. With each degree that our heads flex forward (as we stare at a screen below eye level), the strain on our spines dramatically increases. When an adult head (that weighs 10 to 12 pounds in the neutral position) tilts forward at 30 degrees, the weight seen by the spine climbs to a staggering 40 pounds, according to the study.
How pervasive of a problem is this? According to the study, the average person spends 14 to 28 hours each week with their heads tilted over a laptop, smart phone or similar device. Over the course of a year, that adds up to 700 to 1400 hours of strain and stress on our spines. As a result, the number of people dealing with headaches, achy necks and shoulders and other associated pain has skyrocketed. Trained to address postural changes and functional declines, physical therapists are well-versed in treating this modern-day phenomenon, widely known as “text neck.”
Over time, this type of poor posture can have a cumulative effect, leading to spine degeneration, pinched nerves and muscle strains. Scheduling an appointment with a physical therapist can help people learn how to interact with their devices without harming their spines. The PT will prescribe an at-home program that includes strategies and exercises that focus on preserving the spine and preventing long- term damage.
Exercise is an important part of taking care of our spines as we age, but what we do when we’re not in motion matters, too. So next time you pick up your smart phone or curl up with your e-reader, do a quick check of your head and neck posture. Your body will thank you for years to come.
Content borrowed from PPS, reviewed by Jason Koenigs, PT
Jason Koenigs, PT
Do You Know Your Movement Vital Signs?
Do You Know Your Movement Vital Signs?
Most people think of heart rate or blood pressure when they think of vital signs. It is common to use numbers to quantify health and risk of disease. The American Heart Association encourages people to "know their numbers" referring to blood pressure, blood cholesterol, blood glucose, and weight. However, research is now showing the importance of moving properly for health. Let's take a look at some of the numbers you can use to quantify your movement health: Walking Speed Walking speed has been called the "sixth vital sign" in medical literature recently. It is easy to measure, and takes into account strength, balance, coordination, confidence, cardiovascular fitness, tolerance to activity, and a whole host of other factors. It has also been shown to be predictive of future hospitalizations, functional decline, and overall mortality. Normal walking speed is considered to be 2.6-3.1 mph.
Push Ups - Push ups are popular to build strength, but a recent study found that they can show us a lot about your heart too. Researchers found that men who could do 40 or more consecutive push ups were at a 96% lower risk for cardiovascular disease than were men who could do less than 10. The push up test was also more useful in predicting future cardiovascular disease than aerobic capacity measured on a treadmill.
Grip Strength -Hand grip strength has been shown to be strongly correlated with health. The stronger your hand grip is, the less likely you are to suffer from cardiovascular disease, respiratory disease, COPD, and all types of cancer. In the study, muscle weakness was defined as grip strength <26 kg (57 pounds) for men and <16 kg (35 pounds) for women. Grip strength below these numbers was highly correlated with an increase in disease.
Standing From the Floor - If you can't easily get down on the floor and back up your health might be in trouble, according to a study that looked at more than 2,000 people. The study asked people to go from standing to sitting on the floor and back up with as little support as needed. They found that if you need to use more than one hand to get up and down from the floor that you were 2 to 5 times more likely to die in the next 7 years than someone who can do it with just one hand, or even better, no hands at all.
Moving well is obviously important to overall health and longer life. These tests can give a snapshot of how you're doing. If you're having trouble with any of them, considering seeing a movement specialist - your physical therapist.
Content Credit : APTA PPS TOOLKIT
Photo Credit : RUN 4 FFWPU @ Pexels.com
I Laughed So Hard that Tears Ran Down My Leg.
Kim Johnson, MPT
If you find the title of this rings even slightly true for yourself or someone you know, then physical therapy with a pelvic specialist would be beneficial. A therapist that specializes in the pelvic floor can work with a variety of diagnoses and conditions including: pelvic pain, post-surgical care (post-prostatectomy, post-hysterectomy to name a few), pregnancy and post-partum, and by far the most widespread condition we treat is urinary incontinence.
Incontinence can present itself in a variety of ways, for example, “I only leak when I cough, laugh, or sneeze” or “I just can’t seem to get in the house fast enough when I get home.” The most common types of incontinence are stress, urge or a mix of both.
Stress Incontinence relates to physical stressors which can cause leakage. Stressors include but are not limited to: coughing, laughing, sneezing, lifting, running, changing position, and squatting down. Often times with stress incontinence there is a small volume loss of urine. Stress incontinence is typically a product of pelvic floor muscle weakness or motor dysfunction, and can be treated very successfully with conservative physical therapy.
Urge incontinence occurs when you have a very strong and immediate urge to urinate. Essentially the bladder contracts at the wrong time. Typically with urge incontinence there is a large volume of urine lost, compared to stress incontinence. Treating urge incontinence sometimes requires a combination of strengthening, soft tissue work, habit retraining, and possibly medication intervention..
Many people actually suffer from a mix of both stress and urge incontinence. Your physical therapist will work to provide a thorough physical therapy diagnosis of each individual’s situation, and together with the patient will develop a customized treatment plan based on that patient’s case. The treatment can include strengthening, bladder retraining, manual therapy, breathing work, relaxation, dietary recommendations, and biofeedback. What a person is eating and drinking can play a huge role in continence. For example, caffeine is a bladder irritant. Sometimes just removing most caffeine from a diet can calm the bladder and allow a person to sleep through the night instead of being woken multiple times to urinate. Often time people don’t consume enough water through the day and that also can cause issues. Water will dilute urine, making it less irritating to the bladder wall. This can reduce frequency, urgency and urine leakage.
Time and time again I have had people say that their leakage is “normal.” I would disagree; incontinence is common but definitely not “normal.” Just because you have had a baby or are over the age of 65 does not mean that you should have to deal with incontinence. So many men and women live their lives around their incontinence, and it does not have to be so. Therapy is a non-surgical option, which can be very helpful and liberating. Please seek out one of our Pelvic Floor therapists if you, or someone that you know, is suffering with incontinence.
For more information visit our site at https://www.advancedptsm.com/pelvic-health
Let me give you a helping hand!
By Jen Taber, OT, CHT
Summer is here and we are anxious to participate in our favorite activities! We often don’t think about how big a part our hands play in helping us to do those things we love. Sometimes pain can prevent us from enjoying activities to their fullest, but there are helpful tips that can be incorporated to minimize the symptoms. They are called joint protection techniques.
“Joint protection techniques are ways of doing activities so that the risk of overuse/pain is decreased. These techniques can be included into all activities and will help to reduce the stress on your joints. Joints that have already been weakened by arthritis are at risk of being damaged by stress and strain. Improper use of diseased joints may lead to impaired function and deformity.” (Spectrum Health Joint Protection Techniques handout)
For example, if you enjoy gardening, make sure you are breaking up the tasks or switching activities so that you are not constantly grasping the handles of the shovel or pinching to pull up weeds. This ensures that a variety of muscles are being used and joint surfaces do not become overly compressed and irritated. Adaptations to tools such as enlarged/padded handles or spring loaded options, can decrease stresses on the joints for those who have arthritis to accomplish tasks much easier.
Some people enjoy mowing the lawn but it can also be taxing to the small joints of the hand. Holding onto the handles for long periods of time or the vibration can cause numbness/tingling in the hands. Periodic breaks during an activity like this is important. Also, using anti-vibration gloves may be helpful in reducing the impact to the carpal tunnel area and can be found at a local hardware store or online.
Finally, you should prioritize activities you want to accomplish during the day. Consider how long the activity takes and plan those that are more difficult to do during times that allow you to take breaks. Regardless of the activity, respecting pain is of utmost importance.
Hopefully the tips mentioned above, assist you in completing the activities you have been waiting months to do! SO GET OUT THERE AND ENJOY!
Photo by Zhivko - Pixabay
No Referral Need for PT
By Andy Taber, PT, DPT
It still surprises me how many patients are not aware of the choices they have when seeking medical care, and in particular, physical therapy! As an advocate for my profession, I always try to be proactive in educating and informing patients of their rights when seeking medical treatment.
Under current Wisconsin law, Direct Access allows physical therapists to evaluate and treat patients without a referral from a doctor.
Historically, one of the main barriers between injured patients and proper PT services was the necessity of a doctor’s referral prior to any appointments. This extra step often prevents patients from seeking treatment from a qualified physical therapist. Indeed, each year, over 100 million Americans suffer from wellness and mobility impairments, and yet only 10% actually make their way to a physical therapy clinic. With the implementation of Direct Access, however, the process is streamlining. By placing the power directly into the hands of consumers and clinicians, direct access provides a new avenue through which a patient can receive evaluation and treatment for a host of injuries or conditions.
Put simply, Direct Access grants the patient the ability to “refer themselves” to their desired physical therapist, who may then provide evaluation and treatment without the sign-off of a physician. This may seem like a small deviation from the standard medical referral model, but in actuality, it could potentially have a profound effect on eliminating much of the bureaucratic red tape that the previous referral system was built upon. Some key benefits of this reform are as follows:
1. Direct Access eliminates the burden of extraneous visits to physicians. The referral requirement can cause delays and denials of services provided by physical therapists. These delays in care result in higher costs, decreased functional outcomes, and frustration to patients!
2. It promotes more efficient treatment by eliminating sometimes unnecessary and frequently expensive diagnostic testing, like MRI’s and X-Ray’s.
3. Direct Access can lead to both a better treatment experience and outcome for the client. Patients who visited a physical therapist directly for outpatient care had fewer visits (27%) and lower overall costs on average than those who were referred by a physician while maintaining continuity of care within the overall medical system and showing no difference in health care use in the 60 days after the physical therapy episode.
Direct Access also allows for patients to be treated sooner rather than later. Sometimes, injuries are not addressed until weeks, or even months, after originating. This may be due to patients having a difficult time getting in to see a specialist or reluctance in seeking treatment due to uncertainty on which doctor to see. Have you ever tried to “ride out” pain because you didn’t want to spend the time or money on doctor’s visits, specialists, procedures and medications? There is a better way to manage and treat your pain! In Wisconsin, the Direct Access law allows most people with most insurances to see a physical therapist without a prescription or referral from a doctor.
Physical Therapists are experts on the musculoskeletal system, including:
• Pain from muscle injuries
• Joint pain like arthritis
• Nagging back or neck pain
• Sports injuries
• Recovery from broken bones or fractures
• Post-operative rehabilitation
• Vertigo and other balance issues
• A host of other pain resulting muscle, bone and joint problems.
Physical therapists are also trained to ask the right questions, explore all possible causes, offer a clinical diagnosis and let you know if a customized PT plan is right for you - or if you should seek additional insight from a doctor or specialist. Now, most patients can see a physical therapist the same day of an injury, if desired! Treating injuries sooner will not only help speed up the healing process, but it may also decrease the financial burden of medical diagnoses that linger for longer periods of time. Research has shown that early physical therapy treatment decreases overall medical expenses in the long run, for a particular diagnosis!
If you are currently suffering from a recent injury or a nagging issue that’s been around for several weeks or months, feel free to stop by and speak with one of our therapists at Advanced Physical Therapy and Sports Medicine to determine how we can help you on your road to recovery!
Click here for a complete list of locations and therapists.
Why flip flops may not be the best option for your feet
If you wear flip flops into my clinic you get my ceremonial response!
I take them and throw them out onto the lawn in front of our clinic space …. Seriously I do eventually go out and retrieve them and we have a little laugh. There are however, some sound reasons I dislike the favorite summer footwear of the ladies and gentleman who come to see us.
Many of the patients we see are seeking help for foot and ankle related pain or difficulty wearing certain types of shoes. The flip flop, while being easy to slide on and off and comfortable for our poor foot who has been trapped in a hot restrictive boot all winter, does not offer what a good sandal or supportive shoe offers.
Ask yourself, why do we wear shoes? Our friends who are a part of the barefoot running trend question this all the time. But especially here in the mid-west there are reasons to wear shoes:
1) Protection of the bottom of the foot: the shoe offers an interface between our soft tissues on the bottom of the foot (some have softer than others …. hence the term “tenderfoot “from the westerns of my childhood) and the surface we are walking on. We walk and or run on hot, sharp, uneven or even toxic surfaces. So for this function the flip flop does provide a very thin layer of protection.
2) Protection of the toes and top of the foot: There is a reason folks wear steel toed work boots in industrial settings and why there is the sign in the restaurants: no shoes no shirt no service. Wearing flip flops while mowing the lawn or doing gardening for example, where your foot encounters all kinds of nasty sharp, hot or chemically irritating things is, as my father would say …. “Not real smart. “
3) Sun protection: A recent in-service to our staff by a local dermatologist pointed out that we as therapists should screen for Melanoma (skin cancer) on the toes as well as more common areas such as the ears neck and face. This reminds us to protect the exposed tops of the toes to the dangers of sun exposure, which honestly, I never thought about.
4) Shock absorption: Depending on who you read, 2-5 times your body weight is transferred from the ground through your heel and foot. A cushioned shoe along with a healthy foot and leg absorb much of this shock and dampen it. The flip flop, especially a well-worn one offers very little shock absorbing qualities.
5) Support: Our feet are a complex system of bones, muscles, tendons and the nervous system that senses as well as activates the motors that drive us through life. A proper fitting shoe helps to stabilize the foot and control excess motion by the shape of the shoe, and by controlling the heel bone which is the key that locks and unlocks the foot. The flip flop just sits under the heel; it doesn’t wrap around the heel nor does it control the heel.
6) Lastly in order to hold the flip flop on your foot so it is under the foot when your heel contacts the ground you need to pull down with your toe flexors (this is the flip sound) In a regular shoe or a sandal with heel strap, the sole remains in contact with the bottom of the foot through the swing phase due to the foot being enclosed in the shoe /sandal. This is the only time the toe flexors are on constantly instead of on and off through the gait cycle. This can create a muscle imbalance that can lead to the foot being held in a positon leading to hammer, claw or mallet toes. Also in order to be sure the sole is under the heel at heel contact (the flop sound) a person alters their stride which can impact the entire leg and lower body alignment.
So am I going to tell my patients “You are not allowed to wear flip flops ever?” If I did, I may get run right out of the clinic. Instead I suggest that much like cheesecake and my diet, limit flip flop wear in your shoe wear “diet. “
So if you must wear flip flops here are my suggestions:
1) Choose a hybrid flip flop, one that has a heel strap
2) Use flip flops only for short bouts of walking (across the beach versus hiking down the Grand Canyon)
3) Replace flip flops regularly to maximize shock absorption.
4) Never wear flip flops to do lawn mowing, household cleaning or other more dangerous tasks.
5) Sunscreen tops of toes (don’t grease the bottom of the foot however)
6) Pack a “back up “pair of shoes to switch to at the first signs of heel, arch or toe pain.
7) Limit wear time to short trips. If you are shopping, hiking, or touring; wear a sandal.
References:
Zhang, Xiuli, Max R. Paquette, and Songning Zhang. "A comparison of gait biomechanics of flip-flops, sandals, barefoot and shoes." Journal of foot and ankle research 6, no. 1 (2013): 45.
Salathé Jr, Eric P., George A. Arangio, and Eric P. Salathé. "The foot as a shock absorber." Journal of biomechanics 23, no. 7 (1990): 655-659.
Photo Credit: Composita on Pixabay
#1 Thing You Can do to improve your PT Experience
Dealing with the pain and limited mobility associated with an injury or illness can be stressful for so many reasons. You might have questions like, “How long will I be sidelined?” and “What do I need to do to get better?” Or maybe you’re worried about how you’ll pick your children up from school, walk to the train for your commute or prepare meals for your family.
These are all perfectly normal concerns. Luckily, there are some ways that you can gain control over the situation and ensure that you return to the activities you care most about—especially if physical therapy is part of your plan.
What you can do before your very first appointment—and during physical therapy—to take control of that injury-related stress? First and foremost, it’s important to come prepared for physical therapy. And no, I’m not talking about dressing appropriately and arriving on time (or even better, 15 minutes ahead of your scheduled appointment). That stuff is important, of course, but there’s one thing you can do in the days leading up to your appointment that will set you up for success.
Any guesses? I’m talking about starting a list. What kind of list? Well, every time that you feel pain in the affected area or notice an activity that is harder than it was pre-injury, add it to the list! And the more specific you are, the better. Here’s an example to help drive this point home: Let’s say that you’re recovering from a moderate meniscus tear and you have an appointment with your physical therapist in three days. Take notes on how your knee feels first thing in the morning after you’ve been off your feet. How does your knee react when you stand up from a chair—does it feel unstable? Or do you find that you need to clutch the back of the couch on your way to the bathroom? Sharing each of these details helps your physical therapist understand your limitations beyond the injury printed on your intake form.
Now let’s take that list a step farther and add some details about the activities that you typically participate in on a regular basis. Let’s say that you normally play a weekly round of golf, spend your mornings weeding your garden or meet up with friends for a four-mile walk two evenings a week. These activities have become an important part of your life so let’s make sure that they’re factored into your list, perhaps in the “what you hope to get out of physical therapy” category. Painting a clear picture of how active you are—and what types of activities and sports you participate in—can help your physical therapist design an individualized treatment plan and to better help you on your road to recovery. Have you been to physical therapy lately for an injury? Did you find anything else that helped maximize your time in rehab or that improved communication with your physical therapist?
Borrowed from APTA PPS Toolkit March 2019.
Spring Into Running
Kaitlyn Smith, PT, DPT, LAT
Yes, spring is here!! Yes, we survived another Wisconsin winter! Winter is over...right? We’re all itching to get outside and soak in some Vitamin D, well I know I am at least. What better way to enjoy the outdoors than to go for a jog or run? Yes, I said it, you can enjoy the sun, birds, trees, and flowers while running. BUT before you begin, it is very important to understand the basics of running, in order to prevent injury and set you up for success.
To simplify the mechanics of running, think of a bouncing ball. As the body lands on your foot it enables us to store elastic energy and utilize it in the following step, this is a means of conserving energy rather than utilizing a great amount of muscular force to advance the next step. With that said, there are times such as jumping, accelerating, and running uphill which require significant muscular force generation beyond what our body can store from the previous step. Our job is to put the body in the most optimal position to utilize the maximum potential of our spring-like energy (no pun intended).
When we are walking or jogging on flat ground, the body transmits forces and momentum to the tendons, which return most of that energy to the body in a cycle and repetitive motion. Win/Win if you ask me! The trick is maintaining optimal positioning even when we get tired. Proper running form is fundamental and will aid in preventing injury.
From a number of biomechanical studies, ideal running form requires:
1. Relaxed yet compact arms
2. Balanced forward and upright posture
3. Feet landing directly under your center of mass
4. Stride symmetry
5. Good cadence and low ground contact time
You may be wondering why or how the aforementioned requirements correlate to proper form, increased efficiency, and preventing injury. Let’s delve into more insight on how to understand the meaning behind these.
Relaxed Yet Compact Arms: Sound counter-intuitive? It is possible to relax your shoulders and upper arm musculature while maintaining your elbows in a bent position. Your relaxed shoulders will contribute to rotational flow at the shoulders which also transcends to the hips as well, leading to the “spring-like” energy to propel you forward and make running more efficient. The arms should be compact, meaning a nice bend at the elbow. This bend should position your elbow at an approximate 45 degree angle. If you were to put a penny on the inside of your elbow, it should not fall out as you move your arm back and forth. The more movement of your forearm up and down throughout running, the more your bicep and tricep muscles have to work and use precious energy.
Balanced Forward and Upright Posture: This is what keeps your momentum going forward. I like to begin incorporating this by standing and slightly leaning your entire body forward as if you are on a ski jump (ok maybe not as far forward as the Olympians). You will feel your body want to propel forward and this is how you should feel while running. Additionally, leaning forward will help to facilitate foot-strike directly under your center of mass.
Foot Landing Directly Under Center of Mass: For all you physics fans, I like to use the analogy of a force vector to explain the meaning behind this recommendation. If the foot lands in front of the body, the force travels up through the leg and to the body. The body must then overcome this force, acting against the body, to move forward. Overcoming the force against the body takes extra energy and muscle power to propel. Instead, if the foot lands directly under the body, the force through the leg is transmitted straight up and forward to the body rather than at an angle acting against the body.
Stride Symmetry: Symmetry is incredibly important to decrease risk of injury. Inadequate load distribution between the right and left leg often leads to tendinitis along with other overuse injuries such as IT band syndrome. Despite, often-times runners have asymmetries and are unaware since symmetry is difficult to measure yourself. A trusted professional can measure and analyze your stride length, hip rotation, foot landing, specific muscular strength, and range of motion. Physical Therapists are qualified professionals who can analyze and design a treatment plan to address individual asymmetries. This may include video or visual analyzation, positional and functional muscular strength testing, and specific movement assessments.
Good Cadence and Low Ground Reaction Force: Cadence is the amount of times your feet contact the ground within 1 minute. Each person should find their individual cadence recommendation, which is based on a variety of factors. As a general rule of thumb, efficient running coincides with a high cadence. In order to have a high cadence, the time spent on each foot must be low, thus leading to a low ground reaction force and utilizing our “spring-like” energy. Additionally, ALL of the above recommendations help to achieve a high cadence. Therefore, if you begin implementing one of these recommendations, the others may fall into place as well.
Mind you, establishing and maintaining proper running form does not happen overnight, it will take persistence to develop and maintain good running habits. Quantifying your effectiveness of the above recommendations will bring enormous improvement to your running performance. Whether your goal is running for 15 minutes every day or qualifying for the Boston Marathon, having a reliable support system is strongly recommended.
References
Roberts TJ, Azizi E. Flexible mechanisms: the diverse roles of biological springs in vertebrate movement. J Exp Biol. 2011 Feb 1;214(Pt 3):353-61.
Lyght M, Nockerts M, Kernozek TW, Ragan R. Effects of foot strike and step frequency on Achilles tendon stress during running. J Appl Biomech. 2016; 32:365-72.
Cavagna GA, Saibene FP, Margaria RJ. Mechanical work in running. Appl. Physiol. 1964; 19:249-56.
Cover Photo by Composita of Pixabay