Blogs by Topic:
Why Physical therapy or Occupational therapy:
Choose PT First to save time and money
Are you a smart consumer of Healthcare?
Conditions:
Pain relief without medication
What you need to know about arthritis
Your x-rays and MRIs show us the wrinkles on the inside
A new way to Treat Fibromyalgia
Share your goals; they’re important to us!
Back and Neck Pain:
Best way to get rid of back and neck pain
Essential Exercises for Back pain
Can PT help with Headaches/ Migraines?
Can PT help Back Pain? What we learned from Starbucks
Shoulder:
Prevent and Treat Shoulder Pain
Elbow:
Elbow Tendonitis, a.k.a Tennis Elbow
Wrist/ Hand:
Foot/Ankle:
Why Flip Flops may not be your best option
Pelvic Health:
What is Pelvic Health Physical Therapy
How to stay active during pregnancy
Surgery:
Tips & Tricks to Prepare for Surgery
Stronger going into Surgery, Stronger Coming out.
Common Interventions:
Should I be Stretching or Strengthening?
Seasonal:
A PTs Guide to Snow Shoveling Safety
Winter Safety in Industry: Navigating Cold Conditions with Confidence
Finding your balance in winter
Keeping your arms and hands safe in the Winter
Protecting your joints with summer activities
Information for all of our Green Thumbs
Athletics:
Preventing Pickleball Injuries
Could early specialization be the problem?
Concussion:
Everything you need to know about Concussions
Importance of Baseline Concussion Testing
Running:
Return to Running, Spring Edition
Injury Prevention, do shoes matter?
Orchestra and Performing Arts:
Industrial medicine:
Impact of Athletic Trainers in Industrial Care
Lifting Basics Part 1: Warm-ups, Cool-downs, Strengthening
Lifting Basics Part 2: Safe Lifting Practices ALL Workers Should Know.
Lifting Basics Part 3: Exploring Safe and Effective Lifting Techniques
Lifting Basics Part 4: Effective Ways to Safely Move Objects
Tactical Medicine:
Return to Work Assessment for an Injured Police Officer
Police Support Staff Person of the Year
Things we learned from participating in a mass-casualty simulation
Office:
Getting more activity during your workday
Decrease Fatigue and Reduce Stiffness
Direct Contracting:
Our role in providing exceptional care to the employees of local School Districts
Wellness:
Importance of physical activity
Why you need a PT on your team
The 4 P’s of Energy Conservation
Hidden Aches and Pains caused by Cell Phones
How to decrease the aches and pains brought on by using your phone
Movement Vital Sign, what is that?
You’re never too old to strength train
Improve your mood with exercise, especially during the holidays
Importance of Building Strength
Meet the Team:
Orchestrating Care: Advanced PT at Lawrence University
As the physical therapist serving music students at her alma mater, Amber Lisowe knew what question was coming first. She answered it before it was even asked.
“No, I don’t have any musical skills. None whatsoever.”
Her patients at Lawrence University don’t really care. They are less concerned with any musical predisposition she might share with them and more interested in the skills she brings diagnosing and treating their musculoskeletal issues.
And those issues can be considerable.
“These students are practicing and playing for hours, every day,” said Lisowe. “Imagine being in these athletic positions, using your arms and hands, your back, for that long.”
Her use of the term “athletic” is deliberate.
“There are a lot of similarities between collegiate musicians and their counterparts on the field,” Lisowe said. “Both are passionate, and both deal with injury.”
While Lisowe might deem her history of musical pursuits minimal, her athletic undertakings were anything but. A multisport athlete in high school, Lisowe went on to play basketball at Lawrence. As with many athletes who follow the path toward a career in the medical sciences, Lisowe was familiar with injury.
“At Lawrence, I tore my ACL,” said Lisowe. “Twice.”
The first happened early in her freshman season, a devastating blow but one she was determined to overcome. An ACL tear is a season-ending injury with a rehabilitation period of 9-12 months, but Lisowe was passionate about her sport and getting back to it as quickly as possible.
There’s a period of mourning, Lisowe says, that can last until you’re back on the hardwood. The rehab process means you don’t get back to practicing on the court for a full five months. By this time, any concerns of re-injury were the furthest thing from her mind.
“I’d already done running things in therapy, some jumping and cutting, so by the time you get a ball in your hands, your body just kind of takes over and falls into those routines,” Lisowe said. “When you’re back to playing competitively, your focus has shifted from thinking about the leg itself to the dynamics of the game.”
Lisowe would tear her other ACL in her senior year.
“With the first injury, I knew I could work hard and return for my sophomore season. This time there was no next season for me. Definitely a big thing,” she said.
Those serious injuries led to firsthand physical therapy experiences, which in turn kindled Lisowe’s burgeoning interest in the field. Following Lisowe’s time at Lawrence (she graduated with her Bachelor of Arts from Lawrence in 2014), she went on to earn her Doctor of Physical Therapy degree from Rosalind Franklin University of Medicine & Science. She joined Advanced Physical Therapy soon after to work in their Neenah clinic.
The opportunity for Lisowe to work with Lawrence University Conservatory of Music students happened when LU’s longtime physical therapist, Advanced PT’s Phil Sorensen, looked to cut down on his hours. Lisowe jumped at the chance to return to Lawrence.
“Coming from a smaller town, Lawrence was such a great place for me to find myself,” said Lisowe. “The growth and experiences I had there, the friendships I made, really helped shape who I am today. Athletics got me on campus, but the academics and everything Lawrence offers is what really drew me in.”
Lisowe now finds herself at Lawrence one hour a week, providing physical therapy sessions for her student-patients. She sees a range of musicians—freshmen to seniors, flute to clarinet, oboe to piano—with a variety of orthopedic issues.
“A lot of what I do is helping them to manage their pain, figure out what’s causing it, getting them stronger and finding the best positions to hold their instrument,” she said. “There’s not a certain group of people that appear to be more at risk. I enjoy training and teaching them all.”
Sorensen, who worked with LU’s music students for nearly a decade, describes the experience there as unique.
“There’s just such joy there. These students will walk out of a session and begin playing their horn, and stuff like that. It’s just a really cool atmosphere. It makes you young again.”
Lisowe too recognizes the special nature of the gig, one that gives as much as it gets.
“I just love being back here. I think it was meant to be,” she said. “I love being able to make a difference for such a diverse group of talented individuals.”
Mentioning the variety of students she helps, Lisowe notes the common trait all these musicians possess. And despite being “non-musical,” it’s a characteristic she shares with them, as demonstrated throughout her athletic career.
“They are all very motivated to get better so they can continue doing what they love,” said Lisowe.
Click here to learn more about Dr. Amber and Dr. Phil and the clinics they serve at our Neenah Clinic on Commercial St and Appleton East Clinic on Von Roy Rd in addition to their responsibilities at Lawrence.
Physical Therapy Month Spotlight—Dr. PJ Christopherson, DPT
Dr. PJ and family: Sarah, Cooper, Declan & Micah
It would give us no greater pleasure than to shine the spotlight on EVERY one of our providers in October, otherwise known as National Physical Therapy Month, but that ain’t going to happen.
This is a blog, not a book.
So we are choosing to introduce you to PJ Christopherson, and not just because of what he brings to our practice.
He had us with the first sentence that came out of his mouth.
“Yeah, I really tried to talk myself out of going into the PT profession. Because of my mom.”
Wait, what?
A Shawano native, Christopherson grew up with physical therapy. No, this is not an injury story. His mother, physical therapist Jean Darling, has been a fixture in the community’s health and fitness scene for a lifetime. Suffice to say Christopherson had significant exposure to all things PT.
“My mom lived and breathed physical therapy, so I was around it a lot,” Christopherson said. “But for some reason—and I’m not sure what that reason was—I thought of doing something else. Maybe I just didn’t want to pick something because my mom did.”
Christopherson nevertheless found himself gravitating to the health field. His high school anatomy class was an early inspiration; later, an introductory course on health careers at UW-La Crosse revealed the variety of career opportunities beyond PT that were available to him.
Following completion of the course, a turning point.
“Not sure I’d call it closure, but I had this acceptance that PT could actually be something I could see myself doing,” Christopherson said. “Maybe it was on my radar all along.”
Fast forward, Christopherson would earn his bachelor’s degree in Exercise & Sports Science and then (of course!) his Doctorate of Physical Therapy, both at UW-La Crosse. Newly engaged, Christopherson and his wife Sarah moved to the Milwaukee area, where she attended graduate school and he began his career at a small private physical therapy practice.
Not that he didn’t consider other options, including one at Advanced PT, the very place where his mom practiced and thrived.
“Fresh out of school I actually interviewed with (Advanced PT president and co-founder) Rob Worth for a job,” Christopherson said. “At that point, I felt like branching out a bit, doing my own thing.”
A year later, the couple—he from Shawano and she from La Crescent, MN—had the desire to get back to a smaller community. A job at Advanced PT’s Ripon clinic became available, so the Christophersons found themselves headed right where they hoped they’d be.
Now Clinic Director, Christopherson divides his time serving patients in several capacities. He works with his patients at the clinic on Eureka Street, which also happens to be the near-site clinic for the Ripon Area School District (RASD). Advanced supplies PT services to all RASD employees and is part of the care team delivering high-quality, low-cost care to the district since they recently transitioned to a self-funded health care plan.
The relationship began when the district’s primary care physician needed space. His arrival at 402 Eureka Street resulted in conversations (Advanced PT assists several districts with their healthcare via direct contracts) that led to the establishment of the near-site clinic with a range of providers, part of the district’s overall strategy to reduce costs by offering health services to employees free of charge.
“Being part of this means we can really help people on a community-wide level,” Christopherson said.
Christopherson also finds himself as part of the industrial team at Advanced, providing onsite physical therapy, injury management and rehabilitation services to employees at a manufacturing company in a nearby community.
“With these relationships, we’re more than just a provider of services,” Christopherson said. “We’re part of these communities, growing with them and making them stronger.”
Speaking of growing, the Christophersons are the proud parents of three young children; recently they moved to a larger house to accommodate the needs of the family and the extra space they were looking for. They both love where they live (Sarah is a home health occupational therapist), a beautiful area of closely knit communities with small-town values, thriving and upbeat downtowns, a wide variety of recreational opportunities and the convenience of being close to larger metropolitan areas.
“My Milwaukee friends joke that I live in the middle of nowhere,” Christopherson said. “No way. I live in the middle of everywhere!”
Compared to his Milwaukee experience (he also completed a physical therapy internship with the Milwaukee Brewers, providing orthopedic evaluations for prospects at their spring training facility in Arizona), Christopherson finds his current schedule just as jam-packed, perhaps even more so.
He wouldn’t have it any other way.
“I’m in the clinic four days, then one day a week I’m onsite, so I see a little bit of everything, neck to jaws, knees to ankles to shoulders, vertigo patients,” he said. “If you walk in the door, I will see you for X, Y or Z.”
That ability to treat a wide variety of patients is perhaps a gift from his mother, whose resume is ridiculously robust. The fact that he chose to follow in her footsteps makes her very happy, which has upsides when you have a three, two and one-year-old.
“Mom comes down from Shawano every week to babysit,” he said. “That’s been a game-changer.”
—
To learn more about Dr. PJ and/or the Ripon clinic, click here.
Providing Experiences for the Next Generation of Professionals
Getting people back to what they love is the job of an athletic trainer. Ensuring there are plenty of high-caliber graduates ready to serve active populations is the job of universities and colleges, whose programs provide interactive learning environments that will prepare students to enter the profession.
Advanced Physical Therapy & Sports Medicine (APTSM) plays a vital role in the process.
“It’s important we offer internships and job shadowing opportunities for those on the path to becoming athletic trainers,” said APTSM’s Traci Tauferner. “The field is projected to grow 25% by the end of the decade.”
While there is a broad range of settings for the athletic trainer—physician practices, professional sports, clinics specializing in sports medicine, occupational health, and performing arts, to name a few—the vast majority of graduates will enter the field’s most traditional setting: schools.
That’s where Tauferner started out after earning her athletic training degree at UW-Oshkosh. With a robust resume developed since her graduation—she’s the Director of Industrial & Tactical Medicine at Advanced—Tauferner now devotes time both to her administrative duties as well as to the onsite therapy services she delivers at multiple locations.
Tauferner is committed to bringing attention to industrial athletic training, especially as the need for athletic trainers to prevent, evaluate, manage, and rehabilitate conditions faced by workforces—directly at companies and municipalities—continues to grow.
“Achieving injury prevention and cost control in this day and age for the industries and tactical groups we serve is not just a desired outcome,” said Tauferner. “In many cases, it’s a matter of survival.”
More than 55 Wisconsin companies and organizations utilize Advanced PT’s hallmark program of onsite wellness solutions. APTSM’s dedication to workplace health and safety has contributed to recognition at local, state, and national levels.
That kind of focus includes providing learning opportunities for those interested in pursuing a career in the field, and Tauferner is passionate about students understanding the paths available to them.
“It’s important for us to provide these experiences for the next generation, especially so in the bourgeoning industrial and tactical realms, as fewer than 5% of graduates are going into those sectors,” she said.
The connection between APTSM and Tauferner’s alma mater remains strong, as evidenced by UW-Oshkosh student Cade Littleton’s recent experience.
Littleton, a senior in the Masters of Athletic Training Program, spent the summer working through four specific rotations: clinical, hospital, professional team, and industrial/tactical.
Littleton said a few football injuries (“some hip and shoulder pain, but nothing huge like a blown ACL”) led him to seek treatment. Though his high school didn’t have a traditional athletic trainer, a nearby orthopedic group supplied the small school with a physical therapist, and Littleton found himself fascinated by the PT’s skills.
“I was just very interested in what he did, so much so that I actually job shadowed him for one of my classes,” said Littleton. “That set me on the PT path, but once I got to school and got a little more experience with athletic training, I became drawn to that, to work with a younger and highly active population.”
To meet the requirements of the program, one of Littleton’s rotations had him paired with Tauferner.
“This was actually the third time I had met Traci,” said Littleton. “I met her following a presentation she did on mental health, then at the WATA (Wisconsin Athletic Trainers’ Association) conference this year.”
For two weeks Littleton followed Tauferner’s schedule (“yeah, she starts early”), which included stints with the tactical groups she services.
“It was cool to see the firefighters and police officers and how they handle things at their own facilities,” said Littleton. “It was a lot different than my traditional experiences.”
With those tactical groups, Tauferner gave Littleton the opportunity to do full evaluations; she provided guidance, talking Littleton through treatment options and giving him the chance to “do his own thing.”
“Traci allowed me to do a lot more hands-on than I expected, so that was really cool,” he said.
He also learned about Tauferner’s use of and advocacy for modern cupping techniques.
“Just how she used cupping and explained it so it made sense to the client was very interesting,” said Littleton. “That helped me a lot because I’m still a student trying to figure this stuff out.”
Asked about key takeaways following the rotation, Littleton doesn’t hesitate.
“The experience pushes me to continue to learn, to ask questions, and to demand respect as Traci does.”
Littleton admitted he’d like to replicate the demeanor Tauferner exhibited throughout their time together.
“Traci’s vibe is straight confidence,” said Littleton. “The setting doesn’t matter.”
Summer rotations are complete, Littleton is now working with UW-O’s athletic trainer for 2023 football season. Set to graduate next May, Littleton is currently leaning towards working in the high school or college setting, but he’s not ruling anything out.
“I’m not 100% sure yet,” said Littleton.
If uncertain about his job setting, Littleton expresses a clearer view in the geographic sense.
“I’m up to moving,” he said. “I’m not a huge fan of winter.”
—
If you or a student you know is interested in experiencing what Advanced does every day, contact us today!.
Recreating the Unthinkable: The Stevens Point Mass Casualty Event


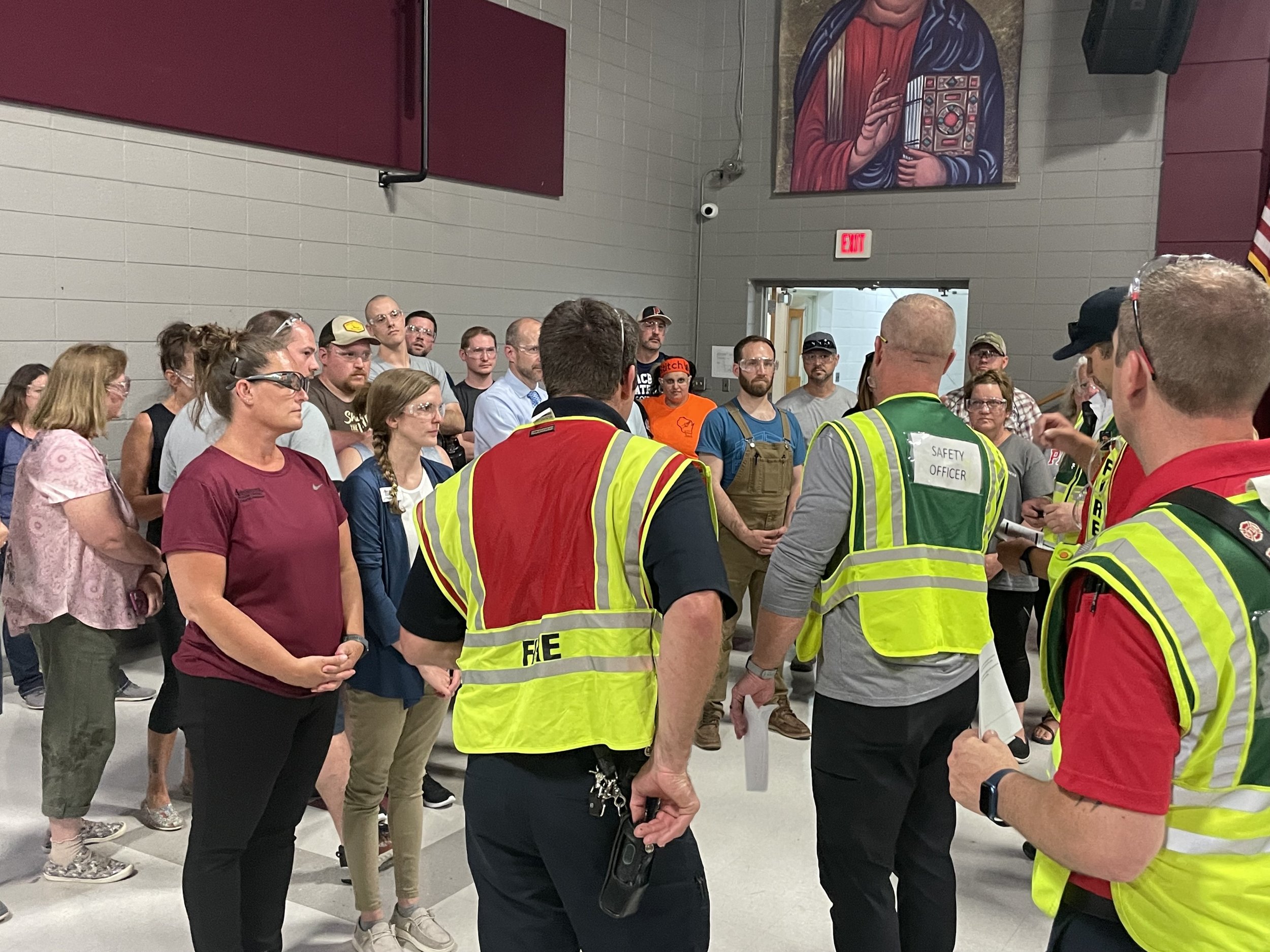

Even when you know it’s a simulation, you’re a bit on edge. Maybe it’s because everyone is.
Or it might be the card they handed you to identify your role in the simulation, which reads “ACTIVE SHOOTER MOCK VICTIM INFORMATION.”
Advanced Physical Therapy’s Lynsey Hansen was ready for her role as a shooting victim nonetheless.
“I was hit but still responsive,” Hansen said. “I just followed what was on the card and did my part.”
The mock disaster, held in Stevens Point for Central Wisconsin first responders, required that exact mindset from everyone involved: be prepared to do your part.
The active shooter event is known as Rescue Task Force Training (RTF). Conducted annually by the Stevens Point Fire Department, Police Department and Emergency Medical Services Team, RTF provides the training ground for multiple agencies to respond to a simulated disaster scenario. The collaborative effort identifies opportunities for enhanced coordination among the agencies tasked with stabilizing a complex situation and triaging victims at a time when every second matters.
While this was Hansen’s first participation in the event as a member of Advanced PT, her boss has been there a few more times.
“Advanced has been working with Stevens Point Police and Fire for 13 years, so this was my 13th,” said Traci Tauferner, Director of Industrial & Tactical Medicine. “I go every year to RTF training, and every year I learn something new.”
Often assisting as a victim in the dress rehearsal, Tauferner recently has taken a step back to view things as an observer.
“As the provider of onsite rehabilitation for Stevens Point Police and Fire Departments, it’s a perfect time for us to educate ourselves about the physical aspects required by personnel to effectively do their jobs in a high stress mass casualty event,” said Tauferner. “With that knowledge, we will understand how we can best rehab them if they have an injury.”
In previous drills, Tauferner focused on her role as victim, viewing the triaging interactions she had with first responders tending to her injuries. This year’s perspective afforded her the opportunity to see department interactions, triage tools, deployment, and the results of public safety partners who have planned and trained together.
Scrutinizing the approach of first responders in managing a large-scale crisis assists Advanced onsite tactical providers.
“We aren’t police officers or firefighters,” said Tauferner. “If we don’t study how they do their work, we won’t understand how to strengthen them, condition them, rehab them, and protect them if they have an injury.”
Hansen, fresh from her first acting stint, appreciated the combined efforts of those who pitched in to coordinate the event.
“You’ve got staff members and groups from multiple locations—Stevens Point, Plover, Portage, etc.—that participate, which is so important because each situation will be unique and you’re going to need to pull from every available area,” Hansen said. “So getting that experience is so beneficial for all parties.”
Afterwards, departments held debriefing sessions, both individually and jointly; those wide-ranging conversations help drive next year’s training. All participants acknowledge the intricacies of fine-tuning the rapid deployment of resources among multiple groups, but their overarching goal is simplicity itself:
To create a unified response that saves lives.
The Journey of Anna Linstedt, LAT
As the chair of the Awards & Scholarships Committee for the Wisconsin Athletic Trainers’ Association (WATA), Anna Linstedt relied on input from the Board of Directors to identify a candidate for the organization’s Distinguished Service Award, given annually to a servant leader in recognition of their dedication to the advancement of the athletic training profession.
“We have a name,” said WATA President Keith Owsley.
Linstedt listened for it. There was a long pause.
“What are you waiting for?” she said.
“I really don’t know how to go about doing this,” he said.
“Just fill out the nomination form, send me a letter, get me their curriculum vitae,” said Linstedt. “It’s not that hard, Keith.”
“Well, we’re nominating the committee chair,” came the response.
The realization that Linstedt herself was the recipient of the award caught her off guard. A question immediately popped into her head; it came out of her mouth almost as readily.
“Don’t you have a better name?” Linstedt asked.
The President answered without hesitation.
*************************************************************************************
The path that led Linstedt to this moment can be traced back to her college days, as one of WATA’s founding fathers was her instructor. He impressed upon Linstedt the vital importance of participating in the association, and she’s been involved ever since, from member to committee leader to regional representative to President, leading the organization from 2020-2022.
The challenges would begin for Linstedt even before she took office, as three weeks prior to the beginning of her term the decision was made to cancel WATA’s annual meeting, the most important event on the calendar and the group’s main revenue generating source.
This would be the first of many disruptions during Linstedt’s unprecedented tenure, but such was the nature of first great pandemic of the 21st century.
Despite the inability to meet in person with lobbyists, state government officials, and even her own staff, Linstedt spearheaded WATA’s effort to achieve their goals, one of which was the streamlining of athletic trainer license requirements.
“That was a huge win for us,” said Linstedt.
Another effort was to gather and present data to lawmakers to ensure reimbursement rates for athletic trainers were equal to those of physical therapists. Working with insurance companies, WATA was able to provide the state legislature evidence from more than 90,000 episodes of care that demonstrated
rehabilitation processes followed by trainers and therapists were the same and should be compensated as such.
“A year later,” rued Linstedt, “this still hasn’t crossed the goal line.”
With the cancellation of the annual meeting and the concomitant reduction in capital, Linstedt and her team needed to go through the budget with a fine tooth comb, determining the absolute must-haves through a process of budgetary triage. Linstedt praised the work done by her predecessors for years of fiscally responsible choices that helped the association to weather the storm that was COVID and still come out in the green.
“The pandemic really forced us to think outside of the box,” said Linstedt.
When asked to reflect on her time at the helm, Linsted wistfully mentioned that a “do over” would be nice.
“There are so many more things we could have done for the association if not for COVID,” she said. “But our focus on advocating for all athletic trainers, in both traditional and non-traditional settings, never wavered.”
Her tenacity as a leader and her journey to athletic training is rooted in her experiences on the playing fields. As a high school freshman, Linstedt was a varsity starter for volleyball and basketball. She ran track as well. And it’s also when she tore her ACL. That very year was the first year Burlington High had an athletic trainer, and she worked diligently to get Linstedt back in the game.
When Linsted returned to her sports the following year, she found herself on the on the bench for JV squads.
“That’s not where I thought I belonged,” said Linstedt.
It was at this point when the school’s athletic trainer took Linsted under her wing, teaching her how to tape and rehab, as well as encouraging the fledgling trainer attend camps over the summers to hone her skills. Linstedt, the kind of athlete who took to sports and made them look easy, was now directing her focus to learning about injuries, keeping athletes healthy, and getting those sustaining injuries back to their sports quickly and safely.
She never went back to high sports as a player. But Linsted’s mentor took her to every football game, every basketball game, wrestling, baseball and track events too. You name it, she was there.
“I became involved in athletics in a different sense,” Linstedt said. “I wasn’t participating, but I was an integral part of our sports programs.”
Linstedt would later attend UW-Oshkosh and complete coursework that included experiences working with athletic trainers in a variety of environments. She also got back into sports as a participant. As testimony to her athleticism, Linstedt was seen “messing around” on a diving board when a lifeguard asked her to try out for the school’s diving team.
“I was never a diver,” said Linstedt.
Nevertheless, she became a collegiate diver.
And as a water skier, she traveled to China to represent the United States in competition.
After earning her degree in exercise fitness management, Linstedt gravitated to the most traditional of settings for the athletic trainer: the high school.
“Even early on, I knew that high school was the place for me,” said Linstedt. “I felt that's where my gifts were.”
She would spend the better part of two decades treating high school athletes. A chance encounter with Advanced Physical Therapy’s Traci Tauferner, Director of Industrial & Tactical Medicine for the Appleton-based group, led to a change in setting that once upon a time would have been unthinkable.
“While I cherish all my time at the high schools, it can be a tough gig for a mom,” said Linstedt.
Tauferner pitched the idea of having Linstedt join her industry team and bring her skill set to a completely different clientele, namely the employees of companies who contract with Advanced to supply onsite injury management services. Linstedt was receptive to the idea of a very different kind of work schedule.
“My kids grew up looking at my calendar,” said Linstedt. “They knew I was going to be missing their activities, that I wasn’t going to be home in time for dinner or to tuck them in at night. I was the only trainer at my school, so I missed a lot of my kids’ events because I couldn’t find anyone to work my time.”
Now a year into her job as industrial onsite provider for Advanced, Linstedt feels comfortable with the transition, using her strengths with the high school athlete and their acute injuries and applying them to a slightly older population who are more often than not dealing with chronic issues. She highlights one important similarity in the treatment of the two groups.
“This goes for everyone, be it a high school athlete or a 47 year old shift worker: each one has to come to the realization that they have to care more about their recovery than I do,” said Linstedt. “I can give you all the exercises in the world to make you better, but if you don’t do them, it’s going to inhibit your recovery. The high school athlete and the industrial athlete have different motivations, but they share same desire for the best outcome, the one that gets them back to the playing field or back to work.”
And Linstedt certainly has no problem relating to the injured workers she sees at multiple industrial sites. In addition to her ACL tear, she’s had multiple shoulder surgeries, ankle issues, and once tore her hamstring off the bone. She understands the sinking feeling that you’re just not going to get through an injury.
“I’m able to use my experiences. I let patients know I understand how they feel, like you’re never going to be able to walk again,” said Linstedt. “But three weeks down the road it’s ‘Look, you’re walking!’ There’s a light at the end of the tunnel. I know. I’ve been there.”
*************************************************************************************
Anna Linstedt received WATA’s Distinguished Service Award on April 23, 2023. A person who prefers not to be called into the light, Linstedt was nonetheless grateful for the award, and very humbled. In her acceptance address, she recognized her husband and family, and now, by removing both the schedule of a high school trainer and the responsibilities of President of her professional organization (oh, but she’s still involved!), she gets to see them with greater regularity.
Clinician Spotlight- Ryan Bailey, PT, DPT.
Meet Ryan Bailey, PT, DPT.
I distinctly heard him say “Central Waters.”
And when a physical therapist gets invited to Amherst, WI to share his expertise, then we’re talking about more than just tapping into the body’s internal mechanisms to relieve pain.
Oooh. Tell me more.
“No, Central Woggers,” he said. “It’s a running group in Amherst. Think the name’s a play on words, a combination of walk and jog.”
Oh, gotcha. I’m guessing this will be more about pain relief than beer.
“Well, those topics aren’t mutually exclusive,” he said.
I like this guy already.
Meet Ryan Bailey, physical therapist at Advanced PT. Recently he was invited to share some of his knowledge with the Central Woggers before they took off for a run.
“So, what topic did they want you to focus on?” I asked.
“Oh, they let me choose,” said Bailey.
Golly, that narrows it down. Bailey’s experience and specialties include working with high-level athletes and orthopedic injuries, foot and ankle dysfunction, pre and post-operative joint replacement and general rehabilitation including ACL reconstruction, sports medicine and biomechanics, just to name a few.
“I decided to give a talk on exercise and pain relief, and why we feel good when we walk and run and exercise,” Bailey said. “More or less about the natural substances within our body to relieve pain that we can tap into instead of relying on medications. Then into anterior knee pain many runners can experience and what the research tells us about strengthening the knee.”
Bailey was under some pressure from the assembled group of several dozen runners to hit the presentation out of the park, as the week prior a nurse and wellness coach named Martha Bailey did just that.
“Yeah, Martha is my wife. She’s pretty good,” said Bailey. “I understand they are inviting her back.”
While he is a frequent runner, Bailey considers running more of a cross training component for some of the many other sports on which he focuses, one of which is surf ski racing. Designed for ocean paddling, surf skis are sit-on top kayaks that are sleek, fast and very tippy. Bailey competed in the sport, a popular pastime with lifeguards, while living in Hawaii and California. Even though it’s tough to find anywhere near the surf ski racing opportunities here in Wisconsin, Bailey still manages to keep his skills sharp.
“There’s actually a very good 17 mile race here called ‘Race the Fox,’ which goes from Berlin to Omro,” he said. “It’s something I’ve done since moving back to Wisconsin.”
Bailey met his Wisconsinite wife in California, where he lived for 30 years, when she went out west for a nursing job. They got married in San Diego and returned to Wisconsin to start their family. They and their three daughters now reside in the house Martha grew up in, located in Fremont. Not surprisingly, their children are into sports and activities just as mom and dad are, and the family takes full advantage of the gamut of outdoor activities Wisconsin has to offer.
And he insists he doesn’t miss the ocean and the beaches.
“I love it here in Wisconsin,” Bailey said. Bailey coaches a number of area teams and is committed to being a resource for youth sports and being there for families after an athlete’s injury. He’s also committed to helping community members stay active and healthy, hence his visit to the Central Woggers.
It seems as if the transplanted Californian has found the perfect place to be.
Learn more here: https://www.advancedptsm.com/ryan-bailey
Quick Access to Quality Care
The Zoom connection was spotty.
“So you said you’re from the Twin Cities? I love Minneapolis,” I stated.
“Not Minneapolis,” she said. “Leopolis!”
Wait, what?
“And now I live in Pella.”
After the reconnect, I had Sally Egan of Advanced Physical Therapy & Sports Medicine (APTSM) begin anew.
“As an onsite provider at three companies and a municipality in Northeastern Wisconsin, it’s my job to help create and maintain healthy environments for employees,” said Egan. “And the best way to do that is to provide quick access to quality care.”
Egan is a veteran of APTSM’s industrial rehabilitation team, a group of licensed athletic trainers and physical therapists dedicated to keeping employees healthy, safe, and on the job. Like many of her colleagues from the athletic training world, she began her career in the high school setting, as the athletic trainer at nearby Shawano High School (about 15 minutes away from what she refers to as the “Twin Cities”) for nearly a dozen years.
She stresses the similarities between the two environments.
“What we do as industrial athletic trainers is bring the sports medicine model of immediate, consistent care to the workplace,” said Egan. “And we do this at no cost to the employee.”
Which is so important to her clients, everyday people who are just trying to make a living and put food on the table.
Egan understands that concept well.
“I grew up in this area on a very small dairy farm. I know what it's like for a family to live paycheck to paycheck and not able to get healthcare when you really should, because you just can't afford it,” said Egan. “So being able to provide that service—literally in my hometown—is just an amazing opportunity for me.”
Interesting that she and her chiropractor brother (“two tiny farm kids”) both pursued careers in health care. It makes complete sense, though, as she describes it as a simple transition from fixing tractors or boards on a wall to fixing people.
The similarities don’t end there, as Egan quickly points out.
“You have to be adaptable and inventive because you don't usually have the resources. That's what onsite rehab is. You don't have a lot of equipment, so you have to work with what you have,” she said.
The companies and organizations she works with rely on Egan to deliver services known as “rapid response,” where direct access to care means employees will be seen in 24-48 hours for an evaluation. That kind of quick care creates the opportunity for an improved healing timeframe, as the onsite provider can swiftly address and manage issues that, if left untreated, could become a recordable injury.
“We can prevent that from occurring,” said Egan. “So you’re keeping the employee healthy and keeping them at their job, and you’re saving the employer money by reducing direct and indirect costs that result from such an injury.”
Again, she leans on her sports medicine background.
“One domain of athletic training is about reactive and emergency care, which in industry is rapid response and OSHA first aid. So we're there for that assessment, and occasionally wound care and emergency care,” said Egan. “For injuries, we’re able to assess and make appropriate decisions if this is something that you can rehab or treat, or make that decision for a proper referral and guide them to where they should go for the best quality and line of care.”
Developing a relationship and a rapport with her employees is crucial.
“Well, it’s on me to get out on the floor and make connections,” said Egan. “You need to show them that you're there to know them as a person, not just a patient.
Forming such bonds requires a level of trust, something Egan says comes naturally when employees get treated right away and feel better. Whether it’s Egan making the rounds on a factory floor or working with a patient who scheduled an appointment in a (usually) small treatment room, the brief interactions are the sources of the best kind of marketing there is word of mouth.
“One employee will say, ‘Sally has done great things for my shoulder. Go see if she can help you.’ And that keeps my days full,” said Egan.
Egan highlights additional services she can provide if companies so choose. One company, for instance, wanted to offer their office personnel some strategies to improve general wellness. So, every week at the scheduled time, staff members stop what they are doing, grab a chair, and join Egan at the center of the office, where she leads them in fifteen minutes of stretching and body mechanics.
“It’s just a special need that the company felt strongly about, and we can do those types of things,” said Egan. “We individualize services based on the company. I meet with HR every single week at my companies just to keep the lines of communication open. We’re there to prevent health issues as much as possible, so that kind of collaboration ensures their needs are being met.”
The stability of the Wi-Fi connection notwithstanding, someone needed to get going. Technically her “day off,” Egan was headed to a side gig, teaching chair yoga to retired adults. But she wanted me to know she hadn’t looked at list of questions I had sent her prior to the interview.
“I wasn’t going to prep for this. Because what works in this field is that we're ourselves. We're not scripted. You get the real me,” said Egan.
The small-town country girl paused, and before signing off acknowledged one final similarity between her job as an industrial rehabilitation specialist and her work with high school athletes in a previous life.
“We’re in healthcare for a reason, and that’s to help people. I get to make those personal connections with industry clients just like I did in sports medicine. And the best part is when I get somebody that comes in and says, ‘Thank you so much for helping me. I feel so much better, and I didn't know if I was ever going to feel better.’
“That’s the best part of my job.”
—
Click Here to learn more about our Industrial and Tactical Medicine and Wellness programs.
Pelvic Health and You
May is Pelvic Health Month and here at Advanced, we are all about changing the narrative around symptoms/conditions that may be caused by pelvic floor dysfunction.
Did you know that 1 in every 3 women will develop a pelvic floor dysfunction in her lifetime and 1 in every 8 men* will develop a pelvic floor dysfunction in his lifetime?
While very common, it’s certainly not normal.
Pelvic floor issues may be embarrassing to admit to and even harder to talk about, but they affect the quality of your life. We understand that you may have questions; that’s why we are here.
Not all physical therapy practices have a therapist who specializes in pelvic pain/dysfunction, but Advanced PT’s Autumn Pawlowski is a physical therapist with training and experience in the management of a wide range of issues (for both women and men) that occur with compromised pelvic floor muscles.
When you are ready, please call the Appleton North clinic (920.991.2561) to request an appointment with Autumn.
In the meantime, here are a few facts that just might be the inspiration for you to take action and get back to living the life you want.
What are pelvic floor muscles?
● Group of muscles in your pelvis that is kind of like a hammock between your sit bones
● Support pelvic organs
● Maintain continence
● Role in sexual function
What happens if there is dysfunction in the pelvic floor muscles?
● Urinary incontinence
● Urinary frequency and/or urgency
● Pelvic pain
● Heaviness/fullness feeling
● Low back or hip pain
Are there other conditions that a pelvic health physical therapist could help out with?
● After a prostatectomy
● Prenatal and postpartum
● Post-cesarean delivery care
What should I expect during my first pelvic health physical therapy visit?
Your pelvic health physical therapist has gone through extensive training in order to treat individuals who have pelvic floor dysfunction.
The first visit will allow you to discuss your concerns with the pelvic health physical therapist and they will ask you follow-up questions.
Then the provider will complete an assessment to help determine the root cause of your symptoms. The assessment may include an orthopedic screen (looking at your back/hips) to see if there are any significant findings that may be contributing to your symptoms.
If the pelvic health physical therapist feels like an internal pelvic floor assessment would be appropriate, they will explain what that would entail. The internal pelvic floor assessment would only be completed if you provide consent. Based on the findings, the pelvic health physical therapist will develop a treatment plan for you.
Treatment may include modifying bathroom habits, modifying diet/fluid intake, strengthening exercises, stretching exercises, breathing techniques, and discussing how the nervous system has a role in your symptoms.
How do I set up an appointment with a pelvic health physical therapist?
You are not alone with your symptoms.
We know how difficult it may be to pick up the phone and call to schedule an appointment, but we promise you you’ll be glad you did. The pelvic health physical therapist will be able to answer a lot of your questions during the first visit.
Call our Appleton North clinic at 920.991.2561 to request an appointment with Autumn Pawlowski PT, DPT.
*Data is limited for our populations that do not align with the above genders; however, we recognize that every population has unique pelvic floor needs and implications.*
References:
The Importance of the Lymphatic System and How We Can Help
Photo caption: OT and Certified Lymphedema Therapist, Allie, teaches our Clinicians about Lymphedema management after surgery.
What is the Lymphatic System?
The lymphatic system is a part of our body that helps keep us healthy.
This system is made up of lymph nodes, lymph vessels, and lymphatic organs, like the spleen and thymus gland. Lymph is a clear fluid that flows through the lymphatic vessels and is filtered by the lymph nodes. It's like a network of tiny tunnels and filters that help remove germs and waste from our bodies.
When germs and other harmful substances enter our bodies, they can get trapped in the lymphatic system. The lymph nodes filter out these harmful substances, like bacteria, viruses, and cancer cells. They also produce special cells called lymphocytes that help fight infection and disease.
Sometimes, the lymphatic system can become blocked. This condition is called lymphedema. Lymphedema can cause swelling in the arms or legs and can be caused by things like surgery, radiation therapy, or infection.
How can We Help?
Connecting with a physical therapist, occupational therapist or Certified Lymphedema Therapist can help manage lymphedema.
These practitioners can design exercise programs that help move lymphatic fluid out of the affected area, reduce swelling, and improve the range of motion.
They may also use techniques like manual lymphatic drainage massage, compression bandaging, and skin care to manage the condition— In these situations, it may be best to connect with a Certified Lymphedema Therapist to discuss this further.
In summary, it's essential to take care of our lymphatic system so it can keep us healthy. We can do this by eating a healthy diet, exercising enough, avoiding injuries that could damage the lymphatic system, and practicing good hygiene. If we do develop lymphedema or other lymphatic system disorders, it’s best to connect with a trained provider that can help manage the condition to reduce pain, improve mobility and keep you doing the things you love to do!
Connect with one of our skilled Certified Lymphedema Specialists to learn more:
Occupational Therapist, Allison Salm at our Touchmark location
Physical Therapist, Lara Bleck at our Appleton West location.
Contact us here if you want to schedule a visit with our team.
What is Modern Cupping Therapy?
Modern Cupping Therapy is a form of alternative therapy that has gained popularity in recent years. It involves the use of cups made of glass, silicone, or plastic that are placed on the skin to create suction. This suction is believed to increase blood flow to the area and promote healing.
Cupping therapy has been used for centuries in traditional Chinese medicine, and its modern iteration has evolved to become a non-invasive and safe therapy.
Here's what you need to know about this popular alternative therapy:
How does Modern Cupping Therapy work?
During a cupping session, a therapist places cups on the skin and creates suction. The suction is created using a handheld pump. Once the cups are in place, they are left on the skin for several minutes before being removed. Sometimes, they are moved in a very specific pattern or sequence depending on the desired effect.
The suction created by the cups is believed to stimulate blood flow to the area and promote healing. It can also help to relax the muscles, reduce pain, and improve overall circulation.
What conditions can Modern Cupping Therapy help with?
It can be used to help many different conditions including, but not limited to, those listed below:
Back pain
Neck pain
Shoulder pain
Knee pain
Migraines
Arthritis
Fibromyalgia
Lymphedema
Is Modern Cupping Therapy safe?
Yes! It is generally safe when performed by a qualified healthcare professional. Minor side effects may include mild discomfort, bruising, or skin irritation. It is important to seek the advice of a qualified healthcare professional before using cupping therapy.
Conclusion
Modern Cupping Therapy is a popular alternative therapy that has gained popularity in recent years. It involves the use of cups placed on the skin to create suction, which is believed to stimulate blood flow and promote healing. The therapy is generally safe when performed by a qualified healthcare professional and can help with a variety of conditions. However, it should not be used as a replacement for conventional medical treatment. If you are interested in trying Modern Cupping Therapy, call today and we can chat further to determine if cupping is right for you and how to work it into your treatment program.
References:
Wang, Sz., Lu, Yh., Wu, M. et al. Cupping Therapy for Diseases: An Overview of Scientific Evidence from 2009 to 2019. Chin. J. Integr. Med. 27, 394–400 (2021). https://doi.org/10.1007/s11655-020-3060-y
Mohamed, Ayman A., Zhang, Xueyan, and Jan, Yih-Kuen. ‘Evidence-based and Adverse-effects Analyses of Cupping Therapy in Musculoskeletal and Sports Rehabilitation: A Systematic and Evidence-based Review’. 1 Jan. 2023 : 3 – 19.































